Medical & Prosthetic Case Studies
Custom Made Ergonomic Mattresses and Cushions for the Disabled
Summary: A Dutch manufacturer of custom products for the disabled chose 3D scanning to help produce made-to-order ergonomic mattresses and seat cushions for wheelchairs.
The Goal: To create precise 3D models from scanning vacuum mattresses that clients have either sat on or laid down on. The mattresses are scanned, CAD models are made, and the final mattress or seat cushion is milled.
Tool Used: Artec Leo
A few years ago, Kersten Revalidatietechniek, a Dutch manufacturer of customized products for the disabled decided to expand its business. Kersten was already making high-quality products which allowed persons with limited physical abilities to enjoy life to the fullest. For example, the company was famous for customizing automobiles to give the disabled the autonomy a car can provide.
To expand its product line, the company wanted to begin manufacturing custom mattresses for the disabled: both for the wheelchair and the bed. After doing preliminary research on available technology and designing a manufacturing process, the company chose to purchase an Artec Leo scanner and started work
This is their process:
- A patient arrives at the Kersten facility or a staff member goes to the patient’s home.
- A special vacuum mattress is used.
- A patient lays or sits on this mattress and the air is sucked out. This leaves the mattress in the shape of the individual’s back.
- The mattress is then scanned using an Artec L scanner and the 3D model is imported into VX software (developed by ZW3D). Scanning takes less than 5 minutes and total post-processing time is around 20 minutes for each bed mattress or 10 minutes for a seat mattress.
- In the software, the scanned file is made into a proper CAD file and is ready to be milled.
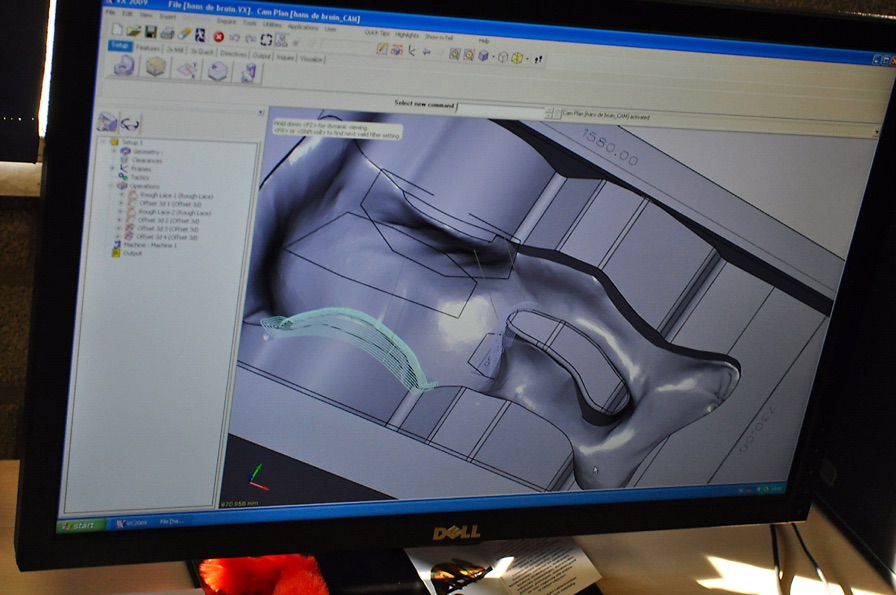
- The CAD model is imported into Eureka software which is used to automatically create a sensible path for the milling machine.
- The model is then milled by a Motoman robot.
To mill a customized mattress takes approximately 1.5 hours.
A Doctor Gives His Patients a Window Into the Future
Summary: To avoid disappointment and even lawsuits, a maxillofacial surgeon needed to show his patients precisely what their faces would look like following surgery.
The Goal: To 3D scan a patient’s face with a handheld 3D scanner, modify the 3D model with the coming changes, and use this model to consult with the patient pre-surgery.
Tool Used: Artec MH
Dr. Andrey Guryanov was the first plastic surgeon in Russia to use Artec 3D scanners in the field of maxillofacial surgery and research. Recently, we had a chance to spend an afternoon with him and learn the ins and outs of his field and how he uses Artec technology.
Dr. Guryanov told us that he has always been fascinated with trying to implement modern technology into the practice of medicine. He stumbled upon Artec almost by accident and was intrigued by a high-tech company that had roots in Russia.
Having purchased a scanner, he and his partner firm, Bonaforma started experimenting. Bonaforma is a software service provider which developed tools to help plastic surgeons visualize the end result of any particular surgery. Moreover, the doctor started using the scanner in his research, trying to pin point reasons for why a patient’s chin sometimes takes a different shape than the shape of the implant. Primarily, though, Dr. Guryanov uses his Artec scanner in the design and development of custom implants, as well as showing expected results to patients. Patients appreciate being involved in the process, while custom implants are superior to the “one-size-fits-all” implants because they better contour the patient’s natural curves and are appropriate in size and form. Moreover, custom implants cause less damage during setting and significantly decrease the risk of displacement after the procedure.
Before working with Artec scanners, the doctor used a “home-made” 3D scanner which consisted of two photo cameras mounted on tripods. This method of digitalization took a lot of time, so often the doctor didn’t even bother with it. Thus, he is most impressed with Artec’s speed of shape acquisition, easy to use software and the fact that the scanner is handheld.
When he first started using an Artec scanner in his daily work, the word spread. Patients heard of this novel method of seeing results before the actual surgery and started to make appointments for consultations. Doctor Guryanov didn’t specifically advertise this technology, but patients found out through word of mouth.
This is Dr. Guryanov’s process:
- Patient comes in for a consult. Doctor explains the procedures in detail. He then scans the patient: a 360 degree scan of the neck, face, chin, and forehead. One scan takes approximately 30 seconds and that one scan is enough.
- Post-processing in Artec Studio takes a few minutes.
- Export of scan into Bonaforma software, where a Bonaforma technician works with the doctor and patient. The patient sees in real time, how his/her face can be changed.
- Using the 3D simulated image, the doctor and patient settle on the specifics.
- Patient is sent to do a CT scan. Every person is different, so the doctor has to know where and how the soft tissue is positioned. This will affect the exact shape of the implant.
- A silicon implant is designed by the doctor and prepared at a lab.
- Surgery
- Post-op check up
Doctor Guryanov, also shared a few stories with Artec.
He was at a professional conference advocating the use of 3D scanning technologies in maxillofacial surgery. Some of his colleagues had reservations about introducing new methodologies into their daily work. One colleague in particular was adamant and proclaimed that 3D scanners are a luxury and good results can be attained without fancy equipment. A few weeks later, a patient of that particular surgeon came to see Dr. Guryanov because she was unhappy with results of her surgery.
Three weeks after surgery, a patient came in with extreme post-op swelling. She claimed that the implant shifted. The doctor hadn’t seen a case like this for many years. It was strange. The doctor sent her for a CT and it appeared that the implant was in its rightful place. After a few days the patient’s swelling went down and it turned out the swelling was caused by a temporary reaction to the silicon implant. “But can you imagine what would have happened had I not modeled the implant before hand and the swelling didn’t go down?” said Dr. Guryanov. “From a legal point of view, I protected myself.”